Melanoma
One would think that our furry friends would be protected from the harmful effects of the sun; however, skin tumors, particularly melanomas, are the most common malignant growths found in dogs.1 Since certain skin cancers, including melanoma and mast cell tumors, can be fatal for your dog, it is important to have your vet examine any unusual growths.1 The good news is that when an overgrowth of these melanin pigment-producing skin cells is detected early, your dog’s skin cancer can often be treated successfully.
Melanoma can be categorized as benign or malignant. Although the risk of metastasis or spreading for the benign form is low, the locally invasive growth can harm normal tissue surrounding the tumor. In contrast, malignant melanomas can be aggressively metastatic and spread to anywhere in the body, particularly lymph nodes, lungs, bones and brain.3 Interestingly, the area of the body where melanoma develops determines its severity. For example, oral melanomas are especially invasive and cause local destruction by infiltrating deep into the bone. Moreover, metastasis occurs in approximately 80% of dogs contracting oral melanoma.4
Surgical excision is the treatment of choice for most melanomas. Complete removal of localized tumors and surrounding tissue often serves as a cure; however, if a malignant melanoma has metastasized to other tissues, the prognosis for your dog is not favorable.5. Chemotherapy has had some success with regard to metastatic melanoma, but due to canine melanoma’s high resistance to chemotherapeutic drugs, this is not an effective option. Another more promising option would be the use of Merial melanoma vaccine which does not prevent formation of the cancerous cells but stimulates your pet’s own immune system to help the body get rid of residual melanoma cells after removal of the tumor.6,7 This treatment is currently only approved for late stage melanoma patients.8 Fortunately, a large number of skin melanomas are benign, but again, any abnormal skin growths should be evaluated promptly. Early detection and treatment are essential for a successful outcome.
Benign overgrowth of cutaneous melanocytes, cells that produce melanin pigment in the skin, give rise to melanomas which are often round, raised, firm and darkly colored. They usually occur on head, toes or back and range from 0.25 to 2 inches in diameter.9 Most malignant forms of melanoma occur in the mouth or mucous membranes even though about 10% may be found in hair-covered regions of the body. They are extremely fast growing and likely to metastasize to organs such as the lymph nodes, lungs, and liver if not detected and treated.1
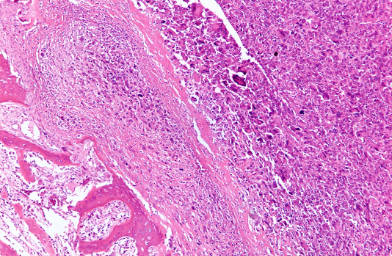
Melanomas with high metastatic potential arise in regions such as oral cavity, scrotum, pads of feet or toenail beds. Unfortunately, detection of malignant melanoma in lung using a radiograph (X-ray) usually indicates that the tumor has spread and infiltrated pulmonary tissue. Swelling of lymph nodes may also suggest malignant metastasis. Accumulation of melanin pigment under skin is characteristic of canine melanoma, although some melanoma tumors lack the darkly pigmented color and are called amelanotic. These are often mistaken for other types of tumors.5
Non-malignant forms of melanoma include melanocytic nevus and melanocytoma. Melanocytic nevus tumors are well-defined, rounded, firm, less than 2 cm in diameter, darkly pigmented, and mobile over underlying tissues. In contrast, melanocytomas are benign tumors originating from the external root sheath of the hair follicle. Dogs below 1 year of age have a propensity for the disease, but dogs between 5-11 years of age have a higher incidence. Eyelids are predilection sites for these particular tumors.10
The majority of malignant melanomas (80-85%) are found in the oral cavity and mucous membrane junctions of lips. Only about 10% of these malignancies arise from haired skin. Head and scrotum are only moderately susceptible to malignant melanomas.9 Malignant melanomas are often subdivided into oral, cutaneous, or uveal (intra-ocular).
Oral Melanoma
Oral melanoma is the most common malignant tumor of skin and usually occurs along gums, lips, palate and less frequently along tongue. This highly malignant melanoma spreads easily to lymph nodes, liver, lungs and kidney which are key sites for metastasis.10 Brown, black or grey lumps or lesions on mouth, tongue, lips or gums should be measured since tumor size is extremely important when considering the stage and prognosis for the disease. Veterinarians usually follow the World Health Organization (WHO) system for staging as follows:4
- Stage I tumor: Diameter is less than 2 cm.
- Stage II tumor: Diameter is 2-4 cm.
- Stage III tumor: Diameter is 4 cm or larger; tumor has spread to lymph nodes.
- Stage IV tumor: Tumor has spread to distant sites.
Oral melanoma symptoms include:11
- Facial swelling.
- Bloody drool
- Foul breath
- Difficulty eating
- Loosened teeth
- Food dropping from mouth
Following a biopsy which is used to confirm that the tumorous growth is melanoma, the staging protocol must be followed in order to fully evaluate the extent of tumor development. Attention should be focused on the following three when assessing oral tumors: Magnitude of local destruction, likelihood of metastasis, and detection at distant sites. Chest X-rays are evaluated for evidence of spread, lymph node samples are collected, and an ultrasound exam is used to screen the abdominal region.4
Cutaneous Melanoma
Toe, foot, nail bed melanoma
This type most often arises in nail bed or on foot pads and initially appears as a discrete mass, a lesion accompanied by pus formation, or a diffuse swelling of toe. It is particularly destructive to the bone and exceptionally painful. As you might expect, lameness is one of the first symptoms. Since nail bed and food pad are susceptible to secondary infections, do not think that the area is simply infected. It is important to visit your vet as soon as you detect these problems. Although the secondary infection can be treated with antibiotics, the swelling and pain will not subside.10
As with oral melanoma, staging of the cutaneous melanoma must be conducted following confirmation with a biopsy. This is an aggressive tumor, and chest X-rays, lymph node sampling, and an ultrasound exam of the abdominal organs are critical for determining the extent of cancer growth [9]. Again, local tumor growth, microscopic migration, and distant tumor growths must all be addressed.
Alert your veterinarian if you notice any of the following symptoms:11
• Swelling of foot or toes
• Discoloration of the toenail
• Malformations of toes
• Loose toenails
Following diagnosis, toe is often amputated with the hope that the patient is cured; however, 30-40 % of these cutaneous melanomas have already spread at the time of detection.9 Discuss the possibility of further treatment with your vet to ensure that metastatic spread is prevented or suppressed.
Haired skin melanoma
As mentioned earlier, the region of skin where melanoma develops significantly influences the tumor’s behavior. For example, certain areas of haired skin grow benign forms of melanoma and are categorized as melanocytomas. They do not usually grow rapidly nor do they spread in a malignant manner. However, it is not safe to assume that all haired skin melanomas are benign.
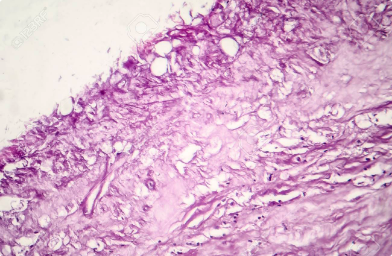
It is important to have all tumors removed and analyzed by a pathologist. Some haired skin melanomas, for example those growing within 1 cm of the mucosal margin such as would be found near mouth, are known to exhibit aggressive, malignant tendencies even if they were not classified as such following microscopic evaluation.4
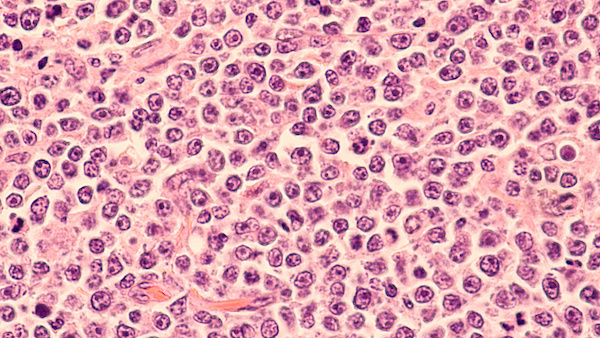
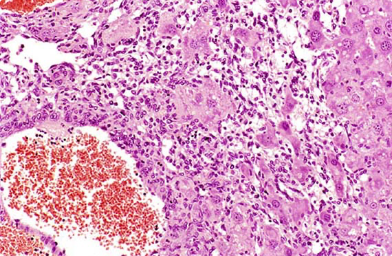
Conversely, melanomas that were classified as rapidly dividing when analyzed under microscope and considered to be malignant, may not behave like malignant growths if monitored over time. The behavior of a given tumor is often evaluated using the mitotic index which is the number of cells undergoing division (mitotic figures) within a microscopic field. If the number of mitotic figures per high power field is less than three, it is assumed that the tumor will behave in a more benign manner. Predictions using microscopic evaluations have become more accurate as stains for certain tissue markers such as Ki-67, a nuclear protein which is strongly associated with tumor cell proliferation and rapid growth, were added to the visualization and quantitation protocols.4
As with the other melanoma forms, all suspicious skin growths with the characteristics listed below should be removed, staged and evaluated for local, microscopic, and distant tumor growth activity.11
- Small blister-like lesions appearing as a rash on the feet, underbelly, or face
- A large dark-colored lump found anywhere on body
- Pain or bleeding from an unusual spot or lesion that is not healing.
Uveal or Intraocular Melanoma
Eye pigments and ciliary body within the eye are particularly susceptible to melanomas. These ocular tumors are often benign and rapid medical attention can reduce the risk for malignant development. Very small growths may not need treatment, but larger ones are surgically removed, treated with laser or removed using local application of intense-cold cryosurgery.10
Ocular melanoma occurs more frequently in female dogs between 5 and 6 years of age and German Shepherds are particularly susceptible. Most of these lesions prove to be benign,.10 and metastasis is not usually a complication with this form of melanoma.4 However, be sure to alert your vet as soon as possible if you notice any of the following symptoms:9
- A dark colored mass in eye or eyelid
- Darkening of iris
- Redness of eye
- Cloudy, dull eyes
- Swelling in or around your dog’s eye
- Muscle twitching around eyes
It is not really clear why skin cancers develop in dogs, especially since their skin is covered with hair and should be protected from the sun. However, ultraviolet light is powerful and can penetrate skin enough to be a factor in tumor development, and as you might guess, the regions where skin cancer often originates are hairless such as around the nose, ears, mouth and lips. Similar to people, numerous factors have been associated with an increased risk for skin cancer and these include excessive sun exposure, chemicals in the environment (carcinogens), hormonal disturbances, and certain viruses. However, similar to human melanomas, a dog’s genetics may be the number one risk factor.6
For example, certain breeds are more vulnerable to certain types of cancer. Doberman Pinschers, Bay Retrievers, Miniature Schnauzers, Airedale Terriers, and Vizslas are particularly susceptible to benign melanocytomas typically when they are between 5 and 11 years old. Schnauzers and Terriers are at the greatest risk for developing malignant melanomas on their toes or in toenail bed, especially if their coat is black in color.1
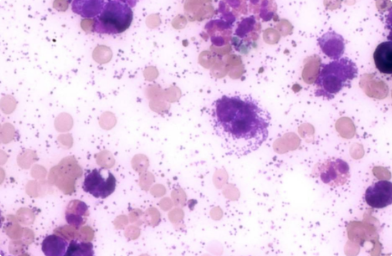
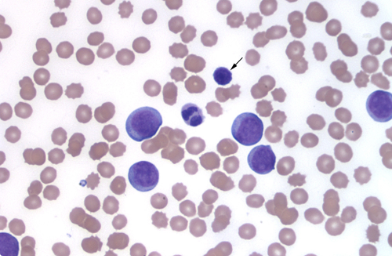
In order to diagnose this disease, your vet will begin with a physical examination which often includes a haircoat analysis, physical reflexes, body temperature, weight, blood pressure, heart rate, respiration rate, breath sounds, pupil reaction time, and oxygen level. Further analysis of the patient’s blood will provide a complete blood count (CBC), serum chemistry profile, platelet count, buffy coat analysis, glucose level, blood urea nitrogen (BUN), liver function panel, packed cell volume (PCV) and a urinalysis.11 CBC and platelet count provide important information about the white blood cell count, platelet number, and the possibility of elevated mast cell counts. Buffy coat reflects a rise in mast cells circulating in blood. Since mast cells do not ordinarily occupy blood in large numbers, a positive buffy coat suggests bone marrow involvement.2
To confirm the diagnosis, a biopsy of the mass will be collected. This involves a fine needle aspirate taken from the growth and sent to lab for analysis. The entire tumor is then removed and submitted for analysis. A pathologist conducts a microscopic evaluation in order to begin to grade the sample by quantifying the number of actively dividing cells or mitotic index. The mitotic index is then used to approximate the tumors potential for invasion and spread to distant sites. Additional tests may include lymph node and/or bone marrow aspirates, x-rays, an ultrasound, or possibly a CT scan with contrast dye to provide a more definitive assessment of the tumor’s metastatic state.5 All of this information helps your vet choose the most promising treatment and provides a possible prognosis for your pet.
Melanoma in dogs is often an aggressive and highly metastatic cancer of the immune system. Unfortunately, by the time it is diagnosed, the tumor has often spread microscopically. Despite complete removal which ensures local control, recurrent metastatic disease is common and additional treatments such as radiation and/or immunotherapy are added to assist the primary treatment.2
The primary treatment depends upon the type of tumor and its location.1. For example, nail bed tumors might be more successfully treated using full amputation of the affected toe due to invasion of bone.10 Although complete surgical removal of the tumor and surrounding tissue may remove threat of the disease, the possibility for metastasis to nearby lymph nodes or other distant sites cannot be ruled out. To ensure the most positive outcome, a CT scan is conducted and a radiation therapy plan is developed for your pet.2
Fortunately, melanoma is quite sensitive to radiation and this option is often used for either local treatment of locations not amenable to surgery, such as bones, teeth, and soft tissues of the upper jaw and tongue, or for more extensive regions of tumor development, particularly lymph nodes or large inoperable melanomas. This approach to controlling the cancer is successful 70% of the time, although recurrence is common.1
Melanomas are most responsive to relatively large doses of radiation applied less frequently. For example, radiation therapy applied once weekly for 3-6 weeks would be a typical protocol.2 Reducing the frequency of treatment allows for normal tissues to heal and decreases the potential for side effects. During the radiation treatment, your dog will be anesthetized. Although sloughing or hollowing of nails or footpad may occur, these tissues will regrow and side effects from treatment are minimal. The median survival time is usually 9 months for either surgery or radiation when used alone.2
In the past, chemotherapy was often used in combination with surgery and/or radiation and carboplatin was considered to be the best choice for optimizing the treatment protocol.10 However, using cytotoxic drugs as a supporting therapy has not been found to be effective in dogs, since canine melanoma is highly resistant to most chemotherapeutics. For example, preventive use of a poly-chemotherapeutic protocol, which involves a combination of cancer-fighting drugs, is simply non-productive. The treatment shows no real benefit to the quality of your pet’s life, nor does it show any significant extension of survival time.8. In fact, current melanoma treatment protocols do not usually include chemotherapy.2
A newer and more promising treatment is immune therapy. This approach uses a vaccine which mobilizes the body’s own immune system to recognize and attack cancer cells. This treatment has significantly improved outcomes and extended survival time;2,7 however, it is currently only administered to dogs with stage II or III cancer. Dogs without cancer cannot receive the vaccine as a preventative therapy.8
Benign tumors that have been removed surgically have an excellent prognosis and your dog may be “cured” of the disease. However, the potential outcome for malignant melanoma depends on the stage of tumor growth when the cancer was first detected and diagnosed.
As mentioned previously, veterinary medicine uses the WHO staging system and if you decide to proceed with surgery and removal of the tumor, the median survival time for your pet with oral melanoma is as follows:4
- Stage I: approximately 17-18 months (with surgery alone)
- Stage II: approximately 6 months (with surgery alone)
- Stage III: approximately 3 months (with surgery alone)
- Stage IV: approximately 1 month (surgery not applicable)
Each type of melanoma may vary from the prognosis listed above. For example, oral melanoma, which comprises approximately 80-85% of all canine melanomas, can be expected to result in the following:
- Untreated dogs survive for approximately 65 days following diagnosis
- Dogs treated with surgery alone have an average survival time of 5-7 months and a one-year survival rate of approximately 21-27%
- A positive response to radiation therapy is experienced by 80% of dogs with oral melanoma with survival times of 211-363 days
- Dogs with advanced stages of oral melanoma that have been vaccinated with Merial vaccine have a survival time of 224-389 days, but this outcome can be significantly improved to 589 days if the primary tumor is also treated with surgery or radiation.
Again, please be aware that early detection of melanoma allows your vet to apply appropriate treatment and perhaps prevent this cancer from spreading. Be attentive to your dog’s health by grooming them regularly, and checking inside their mouth and toes for suspicious dark spots or growths. Your concern and love acts as the number one preventative, since early detection increases your pets’ chances for a long and healthy life.