Precision Medicine
A new approach to medical science made headline news recently when the Precision Medicine Initiative was funded from the President’s 2016 Budget. This novel concept takes medicine away from the one-size-fits-all theme and focuses it on the idea that a condition in one individual is not the same as in another. For example, a treatment that shrinks one patient’s tumor may not work for another diagnosed with the same cancer. This concept can even extend beyond humans and into pets like dogs and cats.
For decades, the search for the “one” mutation or the “one” mechanism driving tumor development captured our attention. Now, a new and exciting advance in cancer research has introduced the notion that there are tremendous differences between tumors across patients. Akin to distinct molecular fingerprints, these individual differences are woven together to form the basis for unique clinical behaviors and drug responses that can be used to develop therapies tailored to each patient. This approach results in a more personalized protocol for clinical treatment and has brought precision medicine to the modern era.
Optimism for Veterinary Oncology
Although veterinary medicine has lagged behind human precision medicine with regard to identifying the molecular mechanisms of cancer, recent studies have provided optimism for both human and veterinary oncology.1 Over the last two decades, efforts to sequence the genomes and to determine abnormal metabolic activities in various animals have provided a much needed tool box for understanding this disease and manipulating its outcome. Although cancer is the leading chronic disease and one of the most common causes of death in companion animals, it remains difficult to define. We could claim that cancer is simply a disease of certain dysregulated genes and metabolic activities; however, each patient diagnosed with the same type of cancer may have very different mutations that trigger different response to treatment. This emphasizes the need to develop treatment that targets specific mutations present in each patient.
Diversity of Gene Dysregulation
To date, many studies have focused on proteins coded from oncogenes, which act as “accelerator pedals” for rapid cell division, or on tumor suppressors, which act as “brake pedals.” Cancers often contain major changes in these driver genes and the subsequent metabolic disturbances may result in loss of the cell’s control over growth and division. In fact, a myriad of altered genes and cell signaling pathways mediate cancer development. Recently, it has become apparent that the complexity of cancer derives from the diversity of this dysregulation, and when individual cells within the same tumor exhibit differences, a particularly difficult challenge emerges with regard to effective treatment.
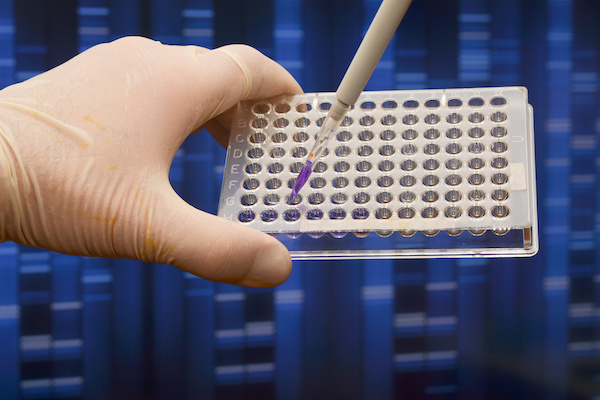
Research strategies have moved from a simple, stepwise evaluation of single pathways or genes to analyzing thousands of genes and pathways in a cancer sample using technologies such as gene array “chips”, next generation sequencing and/or high-throughput assays. The dynamic changes in cancer cells can now be more efficiently monitored and more effective combinations of chemotherapeutic drugs developed.
Matching Drugs to Tumor
Essentially, precision medicine is matching the right drugs to the right patient. For example, finding out that the genetics of certain lung cancers in dogs may be more like human breast cancer rather than other lung cancers was a major breakthrough. Just this year (2019) a study published in Clinical Cancer Research demonstrated that a mutation found in canine lung cancer is similar to a mutation in the human epidermal growth factor receptor 2 (HER2) gene found in women diagnosed with certain breast cancers.2 The HER family of receptors are involved in the regulation of cell growth, survival, and differentiation, which they achieve via their activation of multiple signaling pathways. In fact, the HER2 mutation was found in nearly half of the dogs with lung cancer. This was exciting and led scientists to test the dose/response of the dogs’ tumor cells using Neratinib, a drug commonly used to treat breast cancer in women. Amazingly, the canine tumor cells were exquisitely sensitive to the inhibitory action of the drug, and this result was a key motivator for the first veterinary clinical trial designed to investigate the effect of Neratinib on dogs with naturally occurring lung cancer expressing the HER2 mutation.
It is important to understand that precision medicine includes both target-based and phenotypic drug discovery approaches; however, these two approaches are different. For example, target-based drug discovery (TDD) focuses on finding genetic alterations that can be matched with drugs targeting those genetic changes as described for the HER2 gene above. This approach is at the heart of ‘genomic medicine’, but using genetics alone to fulfill the promise of precision medicine is often insufficient. It is well known that out of a large number of targeted agents prepared for clinical development, only a few act as ‘magic bullets’.
Recent studies suggest that a more powerful approach to precision medicine combines both TDD and functional assays of live cancer cells.4 The drug response of live cancer cells is based on an individual cell’s metabolism and provides the foundation for phenotypic drug discovery (PDD). Using live cancer cells is not only valuable for testing drug sensitivity and responsiveness but can also be quite valuable for predicting the drug resistance of a patient’s tumor.5
PPD has led to the development of new and exciting laboratory methods. These methods have proven to be highly successful for identifying cancer cell types and for determining the sensitivity or resistance of these cells to specific drugs. The results can then be used to rank each drug’s effectiveness. The advantage of screening live cells is that a patient’s own cancer cells can be exposed directly to drug(s). Choosing drug(s) that are the most successful at destroying these particular cancer cells permits veterinary oncologists to confidently recommend the most effective chemotherapeutic treatment for each individual patient—a precision medicine strategy that has far reaching benefits for both pet and vet.
Big Data Translated to Clinical Practice
New tools for investigation have also contributed to reducing the costs that once made veterinary precision medicine extraordinarily expensive. Our ability to dissect and investigate cancer cells has become more refined and affordable; however, our inability to analyze the huge volumes of biological information available represents a drag on clinical progress. Now more than ever, it is essential that mathematicians, biomedical engineers, and computer scientists collecting “Big Data” work together with oncologists to mine and anazlye the biological information. Collaboration and sharing of data will uncover patterns and connections that can be used for translation of the raw biological information into clinical applications. To promote this development, it is essential that pet owners, veterinarians and research scientists work together to make treatment decisions tailored to individual patients. This customization of health care heralds the golden age of personalized veterinary medicine, an approach that holds so much promise for us and our furry friends.

